April 21, 2020
Created Using Covid19Primer.com
Continued Exponential Growth of Research
There were 1646 new COVID-19 research papers and scientific articles published in the past 7 days bringing the total number of papers published to 6140. The exponential growth predicted two weeks ago in this article continues with a 14 day doubling time. Of the 1646 new papers, 94 of them were explicitly referenced in 4500 mainstream news articles. On the social media side, 701 of the papers were shared on twitter through more than 75,000 tweets.
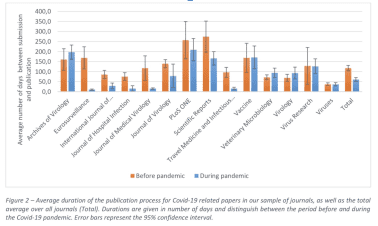
In response to the COVID-19 pandemic, scientific journals are speeding up the peer review process in a bid to get research out to the world quicker than ever before.
Researchers in this paper found that “Compared to articles published in the same journals before the pandemic, turnaround times have decreased on average by 49%,” as you can see from the results below:

Ironically, this research appeared on the BioRxiv preprint server – perhaps because traditional publishing is still not able to move quickly enough.
Drugs, More Drugs and Clinical Trials
Many people are pinning their hopes on a vaccine to allow us to “return to normal”, but this will likely take a long time. Drugs to treat the symptoms of COVID-19 potentially offer us a much quicker path to “return to normal.” There is a large amount of research into drug treatments and as of April 2, 2020 there were more than 300 active clinical trials underway. You can read a summary of some of these clinical trials in an excellent overview published in JAMA by Sanders et al.
Drug discovery and clinical trials research attracted a lot of social media attention this week, with 3 of the top 10 most shared research papers this week focusing on this topic.
HCQ is Not Looking Like the Miracle Drug We Were Hoping For
The third and fourth most shared research papers this week were both on the topic of Hydroxychloroquine (HCQ) and clinical trials. They combined together for over 9000 tweets between those two papers.
The first paper was published by a research team out of China and titled Hydroxychloroquine in patients with COVID-19: an open-label, randomized, controlled trial. The researchers conducted an N=150 person trial in China from mid to late February. It was an open label randomized trial. They found:
- The overall 28-day negative conversion rate was not different between the standard of care (SOC) plus HCQ and SOC group (Kaplan-Meier estimates 85.4% versus 81.3%, P=0.341).
- Negative conversion rate at day 4, 7, 10, 14 or 21 was also similar between the two groups.
- No different 28-day symptoms alleviation rate was observed between the two groups.
Walid Gellad, associate professor of medicine for Pitt General Internal Medicine commented on the results from this paper on Twitter, noting that: “1. The dosage – sky high, but no cardiac adverse events. They were not combining with azithro. 2. No effect on primary outcome (neg conversion rate)”.
The title of the second research paper really says it all: No evidence of clinical efficacy of hydroxychloroquine in patients hospitalized for COVID-19 infection with oxygen requirement: results of a study using routinely collected data to emulate a target trial. This was a trial on 184 French patients. The researchers used “data collected from routine care of all adults in 4 French hospitals with documented SARS-CoV-2 pneumonia and requiring oxygen ≥ 2 L/min to emulate a target trial.” The researchers noted that “These results do not support the use of HCQ in patients hospitalised for documented SARS-CoV-2-positive hypoxic pneumonia.” The caveat here of course is that it was a non-randomized “real world” trial meant to emulate a target trial.
Remdesivir Looks More Promising
Clinical benefit of remdesivir in rhesus macaques infected with SARS-CoV-2. Encouraging research into the clinical benefits of Remdesivir in rhesus macaques monkeys by a team of researchers out of Gilead Sciences (the makers of this drug remdesivir). Their paper, published on the 14th of April, was the 7th most shared research paper this week with 1400+ tweets.
The researchers trialed the drug on 12 monkeys (strangely reminiscent of the plot of the movie by the same name, where Bruce Wills’ character goes back in time to gather information about a nascent plague that is about to exterminate the vast majority of the world’s population…). The researchers “tested the efficacy of remdesivir treatment in a rhesus macaque model of SARS-CoV-2 infection.”
The results were very encouraging and the team found that “day 7 after inoculation, lung viral loads of remdesivir-treated animals were significantly lower and there was a clear reduction in damage to the lung tissue.” The researchers claim that “remdesivir treatment initiated early during infection has a clear clinical benefit in SARS-CoV-2-infected rhesus macaques. These data support early remdesivir treatment initiation in COVID-19 patients to prevent progression to severe pneumonia.”
You can see the impact of the drug on viral load in the lungs of the monkeys in the figure below from their paper.

The research was shared on Twitter by Robert Kruse, MD, PhD where he cautioned that human disease is different “We have 7 day asymptomatic period, albeit lower inoculum.”
The researchers in a different paper note that “ten clinical trials at more than 50 global sites are underway to investigate remdesivir (GS- 5734), an investigational antiviral originally developed by Gilead Sciences to treat Ebola virus infection.”
Finding the Next Miracle Drug Candidate
There is a lot of interesting research going into drug discovery, including these two papers published this week:
A Large-scale Drug Repositioning Survey for SARS-CoV-2 Antivirals. The researchers aim to “identify therapeutics that can be repurposed as SARS-CoV-2 antivirals.” To do this they “profiled a library of known drugs encompassing approximately 12,000 clinical-stage or FDA approved small molecules.” The research team from Sanford Burnham Prebys “reported on the identification of 30 known drugs that inhibit viral replication. Of these, six were characterized for cellular dose-activity relationships, and showed effective concentrations likely to be commensurate with therapeutic doses in patients. These include the PIKfyve kinase inhibitor Apilimod, cysteine protease inhibitors MDL-28170, Z LVG CHN2, VBY-825, and ONO 5334, and the CCR1 antagonist MLN-3897.”

Network Medicine Framework for Identifying Drug Repurposing Opportunities for COVID-19. The research team led by notable network scientist Barabási “predict that the virus can manifest itself in other tissues, such as the reproductive system, and brain regions, moreover we predict neurological comorbidities. We build on these findings to deploy three network-based drug repurposing strategies, relying on network proximity, diffusion, and AI-based metrics, allowing to rank all approved drugs based on their likely efficacy for COVID-19 patients, aggregate all predictions, and, thereby to arrive at 81 promising repurposing candidates.”

In It For Longer. Potentially Much Longer
If we don’t find a successful drug to treat COVID-19 (or a vaccine) then we may be dealing with this crisis for a lot longer than any of us are currently thinking. A research team led by Stephen Kissler from Harvard published research looking at what the next few years of post pandemic life might look like for us. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period.
Kissler et al found that “Intermittent distancing may be required into 2022 unless critical care capacity is increased substantially or a treatment or vaccine becomes available.” The researchers estimated that social distancing measures would need to be in place between 25% to 75% of that time, unless the current critical care capacity of the US was increased. Their models also suggested that under some assumptions social distancing would still need to be in place through until 2024.
The researchers said that “the total incidence of COVID-19 illness over the next five years will depend critically upon whether or not it enters into regular circulation after the initial pandemic wave, which in turn depends primarily upon the duration of immunity that SARS-CoV-2 infection imparts.”
This research was the most referenced research in mainstream media this week with 1296 news articles citing the work. To put this into context, this was the 4th most highly referenced research paper since the start of the outbreak (the most popular research is still this paper from March 10th with 1879 articles referencing it).
We Are Getting Quite Good At Staying At Home
If we are going to be social distancing for longer we should look at how well we are doing it. There has been a lot of research on mobile phone data to track physical mobility, but relatively little looking into how many people we are physically interacting with. There were some new results from researchers at the Department of Demography at UC Berkeley showing that a combination of lockdown and social distancing in the US “are suggestive of a decline in daily interpersonal interaction of about 70% (from an average of about 11 to an average about 3).” You can read the paper here: Quantifying interpersonal contact in the United States during the spread of COVID-19: first results from the Berkeley Interpersonal Contact Study.
Testing
Self Testing Just As Good As The Pros
Self-Collected Oral Fluid and Nasal Swabs Demonstrate Comparable Sensitivity to Clinician Collected Nasopharyngeal Swabs for Covid-19 Detection. “Supervised self-collected oral fluid and nasal swab specimens performed similarly to, if not better than clinician-collected nasopharyngeal swab specimens for the detection of SARS-CoV-2 infection”.
Better Testing With CRISPR
Researchers at the UCSF and scientists at Mammoth Biosciences (who count Jennifer Doudna, a CRISPR pioneer, as one of their advisors) published their research into CRISPR based testing for COVID-19 using samples from nose or throat swabs. The paper published in Nature Biotechnology received mainstream media coverage as it was the first time their technique had appeared in a peer-reviewed journal. One article noted that “One advantage of a CRISPR-based test over a traditional PCR-based test is that it could be run several times on the same sample. This increases the chance of indicating that a negative test truly means a patient does not have the virus.” While STAT news noted that “The test takes roughly 40 minutes, compared with four to six hours for traditional PCR-based Covid-19 tests, which are currently being used.” It should be noted that, at this stage of development, this CRISPR based test may still have a higher false negative than current methods.

The Most Vulnerable Are The Most Susceptible
The wealthiest people in society are able to more effectively shelter in place and limit human interaction, while more vulnerable communities are subject to conditions that are amplifying the spread of the virus. New research looking at a COVID-19 outbreak in a large homeless shelter in Boston found that 36.0% of all the guests residing in the shelter were PCR-positive for SARS-CoV-2. The research illustrates “the rapidity with which COVID-19 can be widely transmitted in a homeless shelter setting and suggest that universal PCR testing, rather than a symptom triggered approach, may be a better strategy for identifying and mitigating COVID-19 among people experiencing homelessness.” The researchers also found that 86% of the people diagnosed with COVID-19 were asymptomatic. This research was the 6th most shared paper of the week with 2400+ tweets.
Jails Act To Amplify The Spread Of The Virus
The Epidemiological Implications of Incarceration Dynamics in Jails for Community, Corrections Officer, and Incarcerated Population Risks from COVID-19. The researchers built a realistic simulation for a jail population interacting with a local community of visitors. They found that: “given a typical jail-community dynamic, operating in a business as usual way will result in significant and rapid loss of life. Large scale reductions in arrest and speeding of releases are likely to save the lives of incarcerated people, staff and the community at large.”
You can see from their results in the figure below the differences between the virus propagating in a jail (left) vs. an urban community (right). It is also important to note that by reducing the spread of the virus in jails, the researchers found that the spread of the virus in the urban community was reduced as well.

Economic Impact
Supply And Demand Shocks: How Different Parts Of The Economy Are Changing In Reaction To The Virus
Supply and demand shocks in the COVID-19 pandemic: An industry and occupation perspective. The researchers from Oxford and the Santa Fe Institute looked at supply and demand shocks and found that “Compared to the pre-COVID period, these shocks would threaten around 22% of the US economy’s GDP, jeopardise 24% of jobs and reduce total wage income by 17%”. Furthermore, they found that at the occupation level “high-wage occupations are relatively immune from adverse supply and demand-side shocks, while low-wage occupations are much more vulnerable.” The research shows that the pandemic will almost certainly unfairly target the poorer members of society.

How Many People Are Actually Asymptomatic
Researchers Are Starting To get An Estimate Of The True Fractions Of Asymptomatic Cases
In Vo, Italy, everyone in the town of 3000 people was tested prior to undergoing a 14 day lockdown. They were then tested again at the end of the lockdown. Researchers found that at the start of the lockdown 2.6% of the population were infected, while at the end of the 14 day lockdown only 1.2% of the town was infected. This result starts to quantify the impact that a 14 day lockdown will have on population infection levels.
Perhaps the most interesting part of the research was that “notably, 43.2% (95% CI 32.2-54.7%) of the confirmed SARS-CoV-2 infections detected across the two surveys were asymptomatic.” Researchers also “found no statistically significant difference in the viral load (as measured by genome equivalents inferred from cycle threshold data) of symptomatic versus asymptomatic infections.”
This asymptomatic number of 43.2% compares with the 86% asymptomatic number found by researchers in the Boston Homeless shelter study referenced above.
Researchers in a different study that was published in the New England Journal of Medicine tested a sample of 215 pregnant women from two hospitals in New York City. They tested them via nasopharyngeal swabs and found that a total of 29 asymptomatic women (13.7%) tested positive for COVID-19 infection. “Thus, 29 of the 33 patients who were positive for SARS-CoV-2 at admission (87.9%) had no symptoms of COVID-19 at presentation,” Dr. Sutton and colleagues wrote. The study had numerous other interesting insights and you can read some of the media coverage here.

These numbers predicting the percentage of asymptomatic cases and those from several other studies were compiled together by Eric Topol and the Scrips Research Center. You can see these in the table that Topol shared on Twitter:

With this data we can now start to estimate that the percent of asymptomatic carriers in the general population. Eric Topol stated on Twitter that “We believe the rate is ~40%.”
Mental Health
Mental health continues to be a big research area for scientists with 115 articles appearing in the topic “Mental Health & Anxiety,” 39 of which were published in the past 7 days.
The paper discussed most in the news was Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science by Emily A Holmes (Karolinska Institutet) et al published in Lancet Psychiatry, which was referenced 43 times, including in the article Coronavirus: ‘Profound’ mental health impact prompts calls for urgent research by BBC. The paper author, Prof Rory O’Connor (professor of Health Psychology at the University of Glasgow) was quoted saying “Increased social isolation, loneliness, health anxiety, stress and an economic downturn are a perfect storm to harm people’s mental health and wellbeing.” Paul Farmer (chief executive of Mind), who is not part of the study, said “While it is too soon to see the extent of the damage, we are hearing that people are already struggling to access the support they need.”
It’s Not Just You, A Lot Of People Seem To Be Suffering
A second paper from a research team out of Italy looked into the different types of impacts on mental health in the general population. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. This research was a web-based survey of 18,147 respondents. The researchers “found high rates of negative mental health outcomes in the Italian general population three weeks into the COVID-19 lockdown measures.” Specifically the respondents highlighted a range of issues including PTSS (37%), depression (17.3%), anxiety (20.8%), insomnia (7.3%), high perceived stress (21.8%) and adjustment disorder (22.9%).
Longer Term Impact Of Viral Infection
In addition to the mental health impacts of being in a pandemic, researchers from the University of California San Diego highlighted the potential of the virus to cause neuropsychiatric symptoms in their recent paper. They say that: “Past pandemics have demonstrated that diverse types of neuropsychiatric symptoms, such as encephalopathy, mood changes, psychosis, neuromuscular dysfunction, or demyelinating processes, may accompany acute viral infection, or may follow infection by weeks, months, or longer in recovered patients.”
Social Media Isn’t Helping Our Mental Health
Research out of China found that there was a “high prevalence of mental health problems, which positively associated with frequent SME (social media exposure) during the COVID-19 outbreak.”
Some Good News
COVID-19 lockdowns cause global air pollution declines with implications for public health risk. Researchers find that “Assuming that the lockdown-induced deviations in pollutant concentrations are maintained for the duration of 2020, we estimate 0.78 (0.09 to 1.5) million premature deaths and 1.6 (0.8 to 2) million pediatric asthma cases could be avoided globally.”

The second order impacts of this pandemic are still being fully understood. We expect a lot more of this type of research to come out over the coming weeks.
And in more good news it looks like there are multiple effective techniques available to decontaminate N95 respirators. The authors outline 4 techniques to decontaminate the N95 masks “UV radiation (260 – 285 nm), 70oC heat, 70% ethanol and vaporized hydrogen peroxide (VHP).” The researchers show that the respirators can be re-used in times of equipment shortage up to 3x with UV or H2O2 vaporization, and up to 2x with 70oC dry heat. However, the researchers show that cleaning the N95 masks with alcohol is not recommended.
Finally some good news for all the health care workers who have to wear N95 masks for long periods of time, leaving them with sores on the face. Researchers are looking into how to alleviate this issue and have published their findings here: Covid‐19: Countermeasure for N95 mask‐induced pressure sore.

Click here to sign up for our weekly briefing.